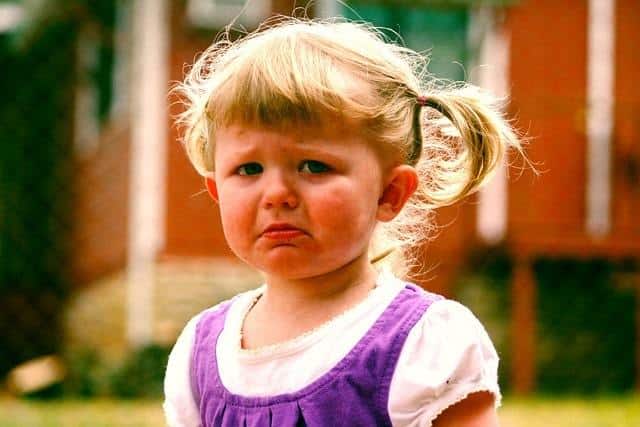
Depression is a type of mood disorder that tends to run in families. [1] When a child or teen has depression, they typically experience extreme sadness and despair. Approximately 5% of children and teens in the US have active depression. [1]
The good news is depression can be treated with anti-depressants and therapy.
Table of Contents
Risk Factors & Causes
Children with learning, attentional, conduct, and/or anxiety disorders have a higher risk of developing mood disorders like depression. Stressful and traumatic events like the loss of a loved one can trigger depression. It can also be triggered by medical conditions, illnesses, disabilities, stressful situations, and parental and romantic relationships.
Moreover, heavy use of social media is associated with depression. [3]
It is important to understand, however, that in some cases, the exact cause of your child’s depression may unknown. [2]
Signs & Symptoms
According to the American Academy of Child and Adolescent Psychiatry, clinical depression is defined as consistently having at least five of the symptoms below for more than 2 weeks. It is important to note that these symptoms must interfere with your child’s daily functioning for him or her to be diagnosed with clinical depression.
Furthermore, if your child or adolescent has two or more symptoms that last for at least a year, but the symptoms are milder and longer-lasting than clinical depression, there is a good chance they are suffering from persistent depressive disorder (also known as dysthymia). [2]
Listed below are signs and symptoms that can present in depressed children and adolescents:
- Feels or appears to be depressed, sad, tearful, and/or irritable
- Loses interest in or pleasure from activities he or she used to enjoy – i.e. hanging out with friends, participating in sports, etc.
- Has a sudden change in appetite causing noticeable weight loss or weight gain
- Experiences a major change in his or her sleeping patterns – i.e. sleeping more or less than normal
- Appears overly energized – i.e. “overly energized”
- Has become more tired (fatigued)
- Has experienced a decrease in energy
- Feels worthless or guilty
- Has a hard time focusing and concentrating, possibly leading to poor academic performance
- Has suicidal and/or self-destructive thoughts or self-destructive behavior [2]
Some depressed children may experience other symptoms along with the traditional symptoms of depression, such as headaches, body aches, or abdominal pain, especially if the child has a hard time expressing their emotions or talking about their feelings.
In addition, some children and adolescents may exhibit their depression through their actions, with irritability and constant complaints of boredom, which may be more noticeable to parents.
Regardless, any talk of suicide or not wanting to be alive needs to be taken seriously and assessed by a mental health professional immediately. [2]
Screening Tools
Some doctors automatically screen children and adolescents for depression at well-child visits. The goal of these screenings is to highlight potential issues. Note: At-home screening tools (i.e. quizzes, assessments, and surveys) should never be accepted as an official diagnosis.
It is highly important that you consult a mental health professional if you suspect that your child is depressed, even if at-home screening tools do not indicate any problems.
Mental health screening tools can be found on the following websites:
- Mental Health America,
- Child Mind Institute Symptom Checker
- Patient Health Questionnaire modified for Teens – used in doctor’s offices
Diagnosis
A combination of clinical screening tools and targeted interviewing by a trained clinician is normally used to diagnosis a child or adolescent with depression.
And, although some primary care physicians (i.e. pediatricians and family medicine doctors) feel comfortable managing pediatric depression, others may refer children and adolescents to behavioral health specialists (i.e. psychologists, clinical social workers, psychiatrists, and/or therapists), especially if the depression is resistant to treatment or there is concern about suicidal thoughts or acts.
Treatment
Therapy and medication are the two most effective ways to treat depression in children and adolescents. Anti-depressants can be prescribed by both primary care providers and psychiatrists. On the other hand, mild depression may be treated with therapy alone. Moderate-to-severe depression is typically treated with a combination of medicine and therapy.
Therapy

Two forms of therapy that have proven effective in the treatment of depressed children and adolescents are cognitive behavioral therapy (CBT) and interpersonal therapy (IPT).
Cognitive behavioral therapy treats your child’s mood by altering the way they think. In other words, it changes their unhealthy thinking patterns. During CBT sessions, a trained therapist uses CBT to help your child properly identify the feelings and moods that are guiding their behavior.
Your child or adolescent also learns how to replace negative thoughts with more positive ones.[2]
Interpersonal therapy, on the other hand, helps to improve your child’s mood by strengthening their interpersonal relationships. During IPT sessions, a therapist helps your child or adolescent identify “interpersonal events” of importance so they can understand how these events are affecting their mood, relationships, and life in general. [2]
*It is important to note that some therapists utilize both CBT and IPT to stabilize depressed children and adolescents.
Family therapy and group therapy are also beneficial for children and adolescents with depression. Family therapy is typically used when dysfunctional family relationships are directly impacting a child or adolescent’s well-being.
Group therapy is typically used to educate the child or adolescent and their family on group dynamics with the goal of helping them better understand this condition. [2]
Medication
Depression is linked to low serotonin levels in the body, so medications like serotonin selective reuptake inhibitors (SSRIs) are sometimes prescribed to depressed children and adolescents to boost these levels. It is common to treat depressed children and adolescents with anti-depressants.
When these medications are carefully monitored and prescribed, they can be very effective in treating depression.
Two FDA-approved SSRIs for children are: [4]
- Fluoxetine (Prozac), which is approved for children 8 years old and older
- Escitalopram (Lexapro), which is approved for children 12 years old and older
In addition, “off-label” SSRIs may be used to treat children and adolescents with depression. “Off-label” means that the medication is assumed to be safe and effective, however, the FDA has not evaluated and approved the medication at that time.
“Off-label” SSRIs sometimes used to treat pediatric depression include: [4]
- Sertraline (Zoloft)
- Paroxetine (Paxil)
- Citalopram (Celexa)
Note: SSRIs are normally prescribed for once-a-day usage. It could take between 4 and 6 weeks before this medicine takes effect.
If your child does not respond to SSRIs, their doctor may prescribe a different class of drugs called “atypical anti-depressants.” “Atypical anti-depressants” can boost your child’s mood by adjusting the amount of neurotransmitters and hormones in their brain. [4]
Examples of “atypical antidepressants” are:
- Venlafaxine (Effexor)
- Desvenlafaxine (Pristiq)
- Duloxetine (Cymbalta)
- Mirtazapine (Remeron)
- Bupropion (Wellbutrin)
Another category of drug often used to treat depression in children and adolescents is tricyclic antidepressants (TCAs). TCAs are considered “older” anti-depressants. As such, these medications usually have more side-effects than current SSRI and “atypical antidepressants.”
Therefore, TCAs are typically not the first medication prescribed to treat depression in children and adolescents. Like “atypical depressants,” TCAs work by adjusting the amount of neurotransmitters and hormones in your child’s brain. [4]
Examples of TCAs are:
- Imipramine (Tofranil)
- Amitriptyline (Elavil)
- Desimpramine (Norpramin)
- Nortriptyline (Pamelor)
- Clomipramine (Anafranil)
Safety & Side-Effects of Anti-Depressants
A major concern of anti-depressants is the risk of suicide. Therefore, there is a “Black Box Warning” on anti-depressants, because it may trigger or worsen suicidal thoughts. However, according to the American Academy of Child and Adolescent Psychiatry, there does not appear to be an increase in suicides while on anti-depressants. [2]
Still, the “Black Box Warning” suggests that anti-depressants should be closely monitored during the first 4 to 6 weeks and whenever the dosage changes.[4]
Regardless, for many, the benefits of anti-depressants far outweigh the risks.
Some of the side-effects of antidepressants include changes in sleep (i.e. insomnia and daytime drowsiness) and gastrointestinal complaints (i.e. nausea, vomiting, constipation, abdominal pain, and diarrhea). The good news is most of the side-effects disappear during the first few months.
As with any medication, it is important to take this medication only as directed. Overdosing on an anti-depressant can be dangerous and even deadly. So, it is extremely important that you read the package insert before giving the medication to your child or adolescent.
And, always ask your child or adolescent’s doctor or pharmacist about possible interactions with other medications, including over-the-counter cold and cough medications. [4]
Outlook

If you have a depressed teen, pay close attention to their behaviors, because depressed teens are more likely to abuse drugs. It is also important to note that a depressed child or adolescent is at risk of having suicidal thoughts, especially if their depression is left untreated. [2]
That is why it is so important to treat depression symptoms as soon as they arise. The good news is treatment can prevent the most serious consequence – suicide.
Resources
- Balanced Mind Parent Network
- Child Mind Institute
- Mental Health America
- National Alliance on Mental Illness
References
- American Academy of Child and Adolescent Psychiatry. (2018). Depression resource center. (2018).
- American Academy of Child and Adolescent Psychiatry. (2018). Depression resource center: Frequently asked questions.
- Child Mind Institute. (2018). Does social media cause depression?
- Understood. (2018). A guide to antidepressant medications.