Many new moms have heard of postpartum depression.
But most are unaware that they may be at risk for other mental illnesses as well.
The risks are real:
13% of pregnant and postpartum women experience anxiety disorders, including OCD. Others will fall into a cycle of substance abuse and addiction.
Unfortunately, due to lack of awareness, most victims never talk about what they are going through, or – worse – their complaints are ignored. These women suffer in silence, and their illnesses are left untreated.
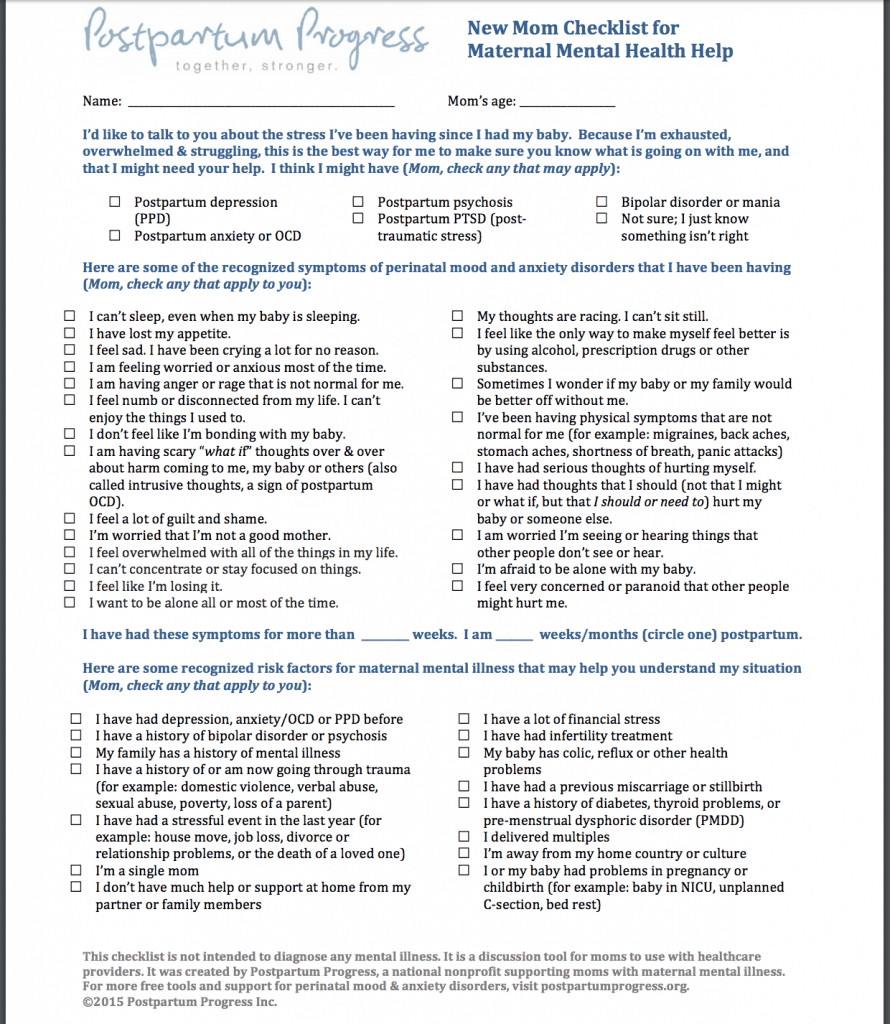
Below is a questionnaire which will help you determine whether you or someone you know should seek the advice of a professional. Click on it to get an enlarged PDF version that you can download and bring to your doctor.
(Click to enlarge, right-click to save to your computer)
Source: postpartumprogress.org
When you are done, read the guide below to find out more about the various mental disorders, how common they are, what the symptoms are, and how they are treated:
Guide to Perinatal Mental Disorders
The sad truth is that postpartum mental disorders–also known as perinatal psychiatric disorders–are extremely common.
Unfortunately, due to lack of awareness, most victims suffer in silence and are never treated.
It’s gotten to the point where the World Health Organization has declared perinatal mental disorders to be a “major global health concern”. (WHO 1)
That’s why we got together with Dr Carla Brock MD FRCPI PhD in order to create this guide with the goal of increasing awareness and giving moms and their families a list of issues to look out for and seek help when needed.
Key point: A large number of women suffer from perinatal mood disorders. However, due to a lack of awareness most victims suffer in silence and are never treated. So if you are a new mom (or know someone who just had a baby) read this guide and seek professional help if needed.
Symptoms of Perinatal Psychiatric Disorders
Perinatal psychiatric disorders can range in severity from sub-threshold to severe psychosis.
There are two main types of women who experience perinatal psychiatric disorders: firstly, women with a history of mental health issues who become pregnant and secondly, women who develop mental health issues in the perinatal period.
Perinatal psychiatric disorders may be classified as:
- Depression
- Anxiety Disorders
- Eating Disorders
- Psychotic disorders
- Drug and Alcohol Misuse.
Things are even more complicated than this classification would suggest as studies show that 2% to 3% of women develop a ‘3-in-1’ diagnosis which involves depression plus anxiety plus stress disorders (Agius).
So rather than sitting at home consulting Dr Google or chatting to family trying to figure out whether your symptoms relate to depression, anxiety or stress disorders (or all ‘three wrapped in one’) just leave it to an expert.
It is also important to have a full medical assessment to rule out other medical conditions such as thyroid disease which can masquerade as depression/anxiety.
The following is an overview of perinatal mental health problems but is not in any way intended to diagnose, treat or substitute for expert medical advice.
Key point: There are different types of mood disorders and proper diagnosis may be complicated. So if you have any suspicion that you may have symptoms relevant to such a disorder, make sure to consult your doctor.
Depression (10-15%)
What is it?
Perinatal depression refers to the presence of symptoms of depression during pregnancy or in the year after delivery of the baby.
Symptoms
Women with perinatal depression frequently experience the following on more days than not:
- a decrease or increase in appetite
- a sense of hopelessness
- feelings of guilt,
- poor concentration
- poor self-esteem
- low energy
- insomnia
- irritability and rage
- excessive crying
- loss of interest
- feelings of sadness or anxiety
Risk factors for development of depression include:
- a prior history of depression
- a family history of depression
- other stressful life events
- poor social support
- serious medical conditions
- substance misuse
- unwanted or unplanned pregnancy
- pregnancy complications
Statistics for pregnant and postpartum women
In general, it is estimated that 10 – 15% of women suffer from perinatal depression. This makes perinatal depression the most common medical complication related to pregnancy.
Specific rates of perinatal depression vary depending on the criteria used to define ‘depression’.
The rate of true clinical depression is 12.7% in pregnancy, 5.7% from birth to two months postpartum and 20% at 12 months. (Gavin).
In contrast, low mood after childbirth, the so called ‘baby blues’ is relatively common and is experienced by 30% to 80% of women. This is usually mild transient and absolutely needs to be differentiated from clinical depression.
When to seek professional medical treatment?
Women who have any concern about symptoms of depression should seek medical help. This is especially the case if there are red flag symptoms such as thoughts about suicide or inability to care for oneself of the baby.s
Reach out for help if some/any of the following persist for weeks or more:
- feeling sad most of the day
- reduced interest in pleasure or interests
- unable to sleep or excessive sleep
- fatigue or loss of energy
- poor appetite or excessive eating
- feeling guilty or worthless
- inability to think
- indecisiveness
- thinking about death
Treatment
There are wide range of treatments available for the management of depression including cognitive behavioral therapy and anti-depressant medications (Marchesi). The risk-balance of taking antidepressants in pregnancy has to be carefully thought through as in general it is usually preferable to avoid unnecessary medication in pregnancy (Pearlstein 2015, Chisolm).For some women the benefits of taking antidepressant medication outweighs the risk of the tablets.
Treatment is tailored to the individual patient and to the stage of pregnancy. While depression in the postnatal period is often self-limiting, it still needs to be appropriately managed.
For more information see our in-depth resource on postpartum depression here.
Key point: Reach out for professional help if you experience any of the symptoms in the yellow box above. There are different types of treatment available. Medications should be carefully managed by a doctor.
While postpartum depression is the best known of the perinatal mental disorders, there is growing recognition that other psychiatric disorders are also common and need appropriate and timely treatment for the health of both mom and baby.
Anxiety Disorders (13%)
What is it?
Anxiety disorders are characterized by excessive worrying that is hard to control, causes distress or impairs function on more days than not (Goodman).
Symptoms
Anxiety disorders usually present with a pervasive sense of worry and irritability. This means that the worry never really goes away. Women may also report physical symptoms such as fatigue or muscle tension.
Risk factors for developing of anxiety are the same as the risk factors for development of depression in pregnancy and the perinatal period. As mentioned above, those are:
- a prior history of anxiety
- a family history of anxiety
- other stressful life events
- poor social support
- serious medical conditions
- substance misuse
- unwanted or unplanned pregnancy
- pregnancy complications
Statistics for pregnant to postpartum women
The rates of anxiety disorders in pregnancy are estimated to be about 13% (Vesga-Lopez). There are a number of sub-classifications of anxiety disorders.
Panic disorders are estimated to occur at a rate of 2% (Ross and McLean, 2008), and fear of childbirth (tokophobia) at 6% (O’Connell).
Perinatal obsessive compulsive disorders are thought to occur at 2% which is double rate of the general population (Russell 2013).
Post traumatic stress disorder is reported to follow childbirth at a rate of 3%.
When to see a professional medical treatment?
It is advisable to seek expert medical advice if any of the symptoms relating to anxiety are making it hard to carry out everyday tasks or if there is any sense that the symptoms feeling of being ‘on edge’ is present much of the time.
Specifically look out for:
- feeling of panic, fear or uneasiness
- heart palpitations
- dry mouth
- nausea
- tense muscles
- inability to relax or sit still
- excessive worry or concern regarding the safety and welfare of baby.
Treatment
A wide range of treatments are available for women with anxiety disorders. The treatment varies according to the severity of the illness, the specific type of anxiety disorder and the stage of pregnancy (Marchiesi).
This may include lifestyle advice e.g. cutting down on drinking coffee and taking regular exercise, enlisting the help and support of family and friends, cognitive behavioral therapy, mind-body therapy like yoga, hypnosis or mindfulness based stress reduction (Bergink).
Medications may be needed for some women depending on the severity of the anxiety (Uguz).
For more information see our in-depth resource on postpartum anxiety here.
Key point: Although less known, anxiety disorders are very common during pregnancy and the postpartum period. Reach out to a professional if you experience any of the symptoms in the yellow box above. There is treatment available.
Eating Disorders (5-7%)
What is it?
Eating disorders are usually defined as a persistent disorder in eating pattern that impairs general health and psychosocial functioning.
Symptoms
The symptoms of anorexia nervosa, avoidance or restrictive food intake, binge eating, bulimia.
Risk factors
Risk factors for eating disorders are poorly understood, although there is some suggestion that genetic and environmental factors may play a role.
Statistics for pregnant to postpartum women
Eating disorders affect 5% to 7% of pregnant women (Easter, 2001).
The rate of anorexia nervosa in pregnancy is just one third of that on the general population as anorexia is associated with sub-fertility. Women with anorexia who do become pregnant usually stop breastfeeding earlier than non-affected woman and have a higher risk of low birth weight babies (Solmi 2014)
Pregnancy can lead to remission from bulimia, but can worsen binge eating disorders.
When to see a professional medical treatment?
It is important to seek help from a medical professional if there are any concerns regarding eating pattern.
Pay special attention to this in the context of somebody who:
- has a known eating disorder
- has a low body mass index
- has hyperemesis gravidarum (excessive vomiting of pregnancy)
- has dental problems due to frequent vomiting
- has associated mood and anxiety disorders, or
- has deranged blood chemistry.
Treatment
Treatment of eating disorders usually involves a multidisciplinary team approach and can involve nutritional rehabilitation, psychotherapy and medication.
For more information see our in-depth resource on postpartum psychosis here.
Key point: Eating disorders can affect the health of both mother and baby. Reach out for professional help if you think you may have an eating disorder, especially if you have any of the symptoms/risk-factors in the yellow box above.
Psychotic Disorders (0.1-0.2%)
What is it?
Psychotic disorders include Postpartum Psychosis, Schizophrenia, and Bipolar Disorder. They involve delusions (fixed false beliefs), hallucinations (false perceptions e.g. seeing or hearing things) and severe impairment in ability to function in the world.
Symptoms
Women with perinatal psychosis such as postpartum psychosis usually present with a sudden onset of severe symptoms such as delusions, hallucinations, confusion and perplexity. These symptoms deteriorate rapidly and tend to fluctuate widely.
Risk factors for developing postpartum psychosis include:
- a history of postpartum psychosis
- a family history of postpartum psychosis
- a personal history of bipolar disorder, schizophrenia, or schizoaffective disorder
- first pregnancy or discontinuation of psychiatric medications during the pregnancy
Statistics for pregnant to postpartum.
Fortunately the overall rates of postpartum psychosis are low, occurring in 0.1% – 0.2% of births. The reason for this is partly that women with existing psychotic disorders such as schizophrenia or bipolar disorders are often less fertile than the general population. There is limited information on the rates of psychotic patients who become pregnant.
When to see a professional for medical treatment?
All women with suspected psychotic disorders need urgent expert medical advice.
Look out for:
- inflated self-esteem
- feeling paranoid/suspicious
- inability to sleep
- being more talkative than usual or feeling pressure to talk
- feeling like your thoughts are racing
- excessive distractibility
- taking excessive risks
Key point: Seek urgent medical advice if you suspect you or someone you know may be experiencing delusions, hallucinations, confusion or perplexity.
Drug and Alcohol Misuse
What is it?
Drug and alcohol use, drug and alcohol use is usually considered as a use of drugs, chemicals or alcohol for recreational purposes.
Symptoms
Drug and alcohol use in pregnancy can present in a wide variety of ways.
The CRAAFT screening score is sometimes used to assess people for their risk of drug or alcohol use. It consists of a series of six questions.
Answering yes to two or more of these questions raises concerns for drug or alcohol misuse.
- Car: Have you ever driven in the same car or driven yourself while under the influence of alcohol or drugs?
- Relax: Do you use alcohol or drugs to relax?
- Alone: Do you use alcohol or drugs alone?
- Annoyed: Have family or friends annoyed you by telling you you need to cut down on your alcohol and drugs?
- Forget: Do you ever forget things because of using alcohol and drugs?
- Trouble: Have you ever been in trouble from using alcohol and drugs?
Risk factors
Women with a prior history of alcohol or drug use are especially vulnerable during the perinatal period.
Statistics for pregnant to postpartum women
About 40% of women drink during pregnancy. Only a very small percentage drink excessively during pregnancy.
High levels of alcohol intake during pregnancy are associated with a fetal alcohol syndrome, which is characterized by impaired growth, abnormal facial features, and abnormalities of the central nervous system.
All drugs/chemicals can affect the developing baby especially if the drugs cross the placenta. This means that the developing fetus is exposed to the same drugs as are circulating in the mom’s blood.
The drugs can also be excreted into the breast milk. This means that drug use even after delivery can still pose a risk to the newborn baby.
Intravenous drug use poses a risk to both mom and baby of blood borne viruses such as HIV and hepatitis B.
Both drug and alcohol use can pose a risk to the mom baby’s safety in the car and at home.
When to see a professional medical treatment?
Any moms with a history of alcohol or drug misuse or suspected of recreational drug use/addiction need to be referred to an expert center for a multidisciplinary approach.
Treatment
The treatment for drug and alcohol dependence varies from person to person. Treatment options also factor in whether or not the woman other mental health disorders such as depression or anxiety.
Key point: Speak to a professional if you have a history of alcohol or drug misuse, or if you find yourself answering ‘yes’ to 2 or more of the questions in the yellow box above.
Complications For The Baby

Perinatal psychiatric disorders affect both mothers and their babies.
Recognized complications for the baby include developmental delay, physical and mental problems (Grote, O’Connor, Howard).
The potential effects of maternal psychiatric disorders on the baby are not limited to the early years of life but can extend right into adulthood.
Information is emerging on the link between perinatal mental health and a wide range of conditions such as:
- antenatal hemorrhage
- preterm delivery
- excessive crying
- behavioral problems
- sleep disturbance
- asthma
- impaired growth
- diabetes mellitus
- and even the sudden infant death syndrome (Grote, Howard).
A number of mechanisms have been proposed to explain the link between maternal mental health and the well-being of the fetus and baby including:
- shared genetics
- exposure of the fetus to high circulating stress hormones from the mother
- impaired maternal immune responses
- poor nutrition
- lack of exercise
- substance misuse
- poor adherence to prescribed therapies
- side effects of prescribed medication and
- lack of interaction between mom and baby.
Perinatal psychiatric disorders affect the baby as well. These effects are not limited to the early years of life but can extend right into adulthood.
Not Enough Women Seek Help

Women who experience psychiatric symptoms during pregnancy or childbirth may be slow to seek care for a number of reasons such as:
- fear of stigma of a psychiatric diagnosis
- fear of loss of custody of the baby
- inability to recognize the need for help due to poor reasoning skills or decision making that can be part of mental health disorders and
- a lack of knowledge by the mother that perinatal mental health affects the baby.
Sadly, the woman who rushes to the doctor with physical symptoms in order to safeguard the health of the fetus/baby may well suffer in silence with mental symptoms.
In fact, it is estimated that 50% of women with perinatal depression remain undiagnosed.
One of the most common barriers to seeking appropriate help for perinatal mental health problems is being unsure about what constitutes an acceptable adjustment to pregnancy/motherhood versus a true psychiatric disorder.
The transition to motherhood involves many changes such as alterations in body shape, lack of sleep, fluctuations in hormone levels and concern over this new little bundle of joy. This is all very normal and natural. However some woman experience more severe symptoms that need expert care to support the optimal longterm well-being of mom and baby.
Where is the tipping point between a sleep deprived mom who just needs a nap versus a mom with full-blown depression?
How can you differentiate between a mom’s intuition that something is wrong with her baby versus an obsessive-compulsive overanxious mom?
You can’t and you shouldn’t even try.
The very last person who should try to diagnose mental health conditions is the affected person. Equally this is not something for family or friends. If you have any concerns about perinatal mental health, then seek professional advice. It is just too important to risk getting wrong.
A study showed that 83% of woman with significant symptoms of depression/anxiety consulted family and friends for help and 66% of woman disagreed with their social support person about the diagnosis (Henshaw).
The best (and only) person to assess the mental health state of any woman in the perinatal period is an experienced healthcare professional who can objectively combine clinical skills and validated questionnaires to differentiate between the acceptable adaptation to the changes of pregnancy/early motherhood versus a psychiatric disease.
It is estimated that 50% of women with perinatal depression remain undiagnosed. Don’t be one of those women. If you suspect you might have any of the disorders on this page, see your doctor as soon as possible.
Final Notes
It would be unfair not to mention the ‘forgotten parent’. Fathers are not immune to pregnancy and postpartum psychiatric disorders and can also experience perinatal mental health issues . Emerging studies suggest that paternal mental health also affects the well-being of the baby (Gentile).
Increasingly and appropriately we are moving from a ‘mom and baby’ entered approach to perinatal mental health to a more holistic integrated family centered approach.
Essentially everyone deserves and needs good mental health.
The bottom line is that anyone with concerns about mental health should avail of expert professional help as there is ‘no health without mental health’. (WHO 2)
References
- Agius A, Xuereb RB, Carrick-Sen D, Sultana R, Rankin J. The co-existence of depression, anxiety and post-traumatic stress symptoms in the perinatal period: A systematic review. Midwifery. 2016 May;36:70-9. doi: 10.1016/j.midw.2016.02.013. Epub 2016 Mar 4. Review.
- Bergink V, Rasgon N, Wisner KL. Postpartum Psychosis: Madness, Mania, and Melancholia in Motherhood. Am J Psychiatry. 2016 Dec 1;173(12):1179-1188. Epub 2016 Sep 9. Review.
- Chisolm MS, Payne JL. Management of psychotropic drugs during pregnancy. BMJ. 2016 Jan 20;532:h5918. doi: 10.1136/bmj.h5918. Review.
- Easter A, Bye A, Taborelli E, Corfield F, Schmidt U, Treasure J, Micali N. Recognising the symptoms: how common are eating disorders in pregnancy? Eur Eat Disord Rev. 2013 Jul;21(4):340-4. doi: 10.1002/erv.2229. Epub 2013 Mar 14.
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005 Nov;106(5 Pt 1):1071-83. Review.
- Untreated perinatal paternal depression: Effects on offspring.
Gentile S, Fusco ML. Psychiatry Res. 2017 Jun;252:325-332. doi: 10.1016/j.psychres.2017.02.064. Epub 2017 Mar 2. Review. - Goodman JH, Chenausky KL, Freeman MP. Anxiety disorders during pregnancy: a systematic review. J Clin Psychiatry. 2014 Oct;75(10):e1153-84. doi: 10.4088/JCP.14r09035. Review.
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010 Oct;67(10):1012-24. doi: 10.1001/archgenpsychiatry.2010.111
- Henshaw E, Sabourin B, Warning M. Treatment-seeking behaviors and attitudes survey among women at risk for perinatal depression or anxiety. J Obstet Gynecol Neonatal Nurs. 2013 Mar-Apr;42(2):168-77. doi: 10.1111/1552-6909.12014. Epub 2013 Feb 1.
- Kimmel MC, Ferguson EH, Zerwas S, Bulik CM, Meltzer-Brody S. Obstetric and gynecologic problems associated with eating disorders. Int J Eat Disord. 2016 Mar;49(3):260-75. doi: 10.1002/eat.22483. Epub 2015 Dec 29. Review.
- Marchesi C, Ossola P, Amerio A, Daniel BD, Tonna M, De Panfilis C.Clinical management of perinatal anxiety disorders: A systematic review.
J Affect Disord. 2016 Jan 15;190:543-50. doi: 10.1016/j.jad.2015.11.004. Epub 2015 Nov 4. Review. - O’Connell MA, Leahy-Warren P, Khashan AS, Kenny LC, O’Neill SM.
Worldwide prevalence of tocophobia in pregnant women: systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2017 Mar 30. doi: 10.1111/aogs.13138. [Epub ahead of print] Review. - Pearlstein T. Depression during Pregnancy. Best Pract Res Clin Obstet Gynaecol. 2015 Jul;29(5):754-64. doi: 10.1016/j.bpobgyn.2015.04.004. Epub 2015 Apr 17. Review.
- Pearlstein T. Use of psychotropic medication during pregnancy and the postpartum period. Womens Health (Lond). 2013 Nov;9(6):605-15. doi: 10.2217/whe.13.54. Review
- Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: A systematic review. J Clin Psychiatry. 2006 Aug;67(8):1285-98. Review.
- Russell EJ, Fawcett JM, Mazmanian D. Risk of obsessive-compulsive disorder in pregnant and postpartum women: a meta-analysis. J Clin Psychiatry. 2013 Apr;74(4):377-85. doi: 10.4088/JCP.12r07917.
- Solmi F, Sallis H, Stahl D, Treasure J, Micali N.Low birth weight in the offspring of women with anorexia nervosa. Epidemiol Rev. 2014;36:49-56. doi: 10.1093/epirev/mxt004. Epub 2013 Sep 11. Review.
- Uguz F Pharmacotherapy of obsessive-compulsive disorder during pregnancy: a clinical approach. Rev Bras Psiquiatr. 2015 Oct-Dec;37(4):334-42. doi: 10.1590/1516-4446-2015-1673. Review.
- Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008 Jul;65(7):805-15. doi: 10.1001/archpsyc.65.7.805
- Vignato J, Georges JM, Bush RA, Connelly CD. Post-traumatic stress disorder in the perinatal period: A concept analysis. J Clin Nurs. 2017 Mar 15. doi: 10.1111/jocn.13800. [Epub ahead of print] Review.
- https://www.who.int/mediacentre/factsheets/fs220/en/ www.who.int/mental_health/prevention/suicide/perinaral_depression_mmh_final.pdf
You may also like: